
Your pancreas is a busy organ that maybe doesn’t get the props it’s due. It’s your body’s insulin producer, the hormone that regulates your blood sugar.
For people with high-sugar diets, the pancreas can end up working overtime by shooting out more and more insulin. Over time, the body can start resisting its own insulin as those receptors get worn out. That’s called type 2 diabetes, and once it’s developed it usually needs to be managed for the rest of your life with diet changes and insulin injections.
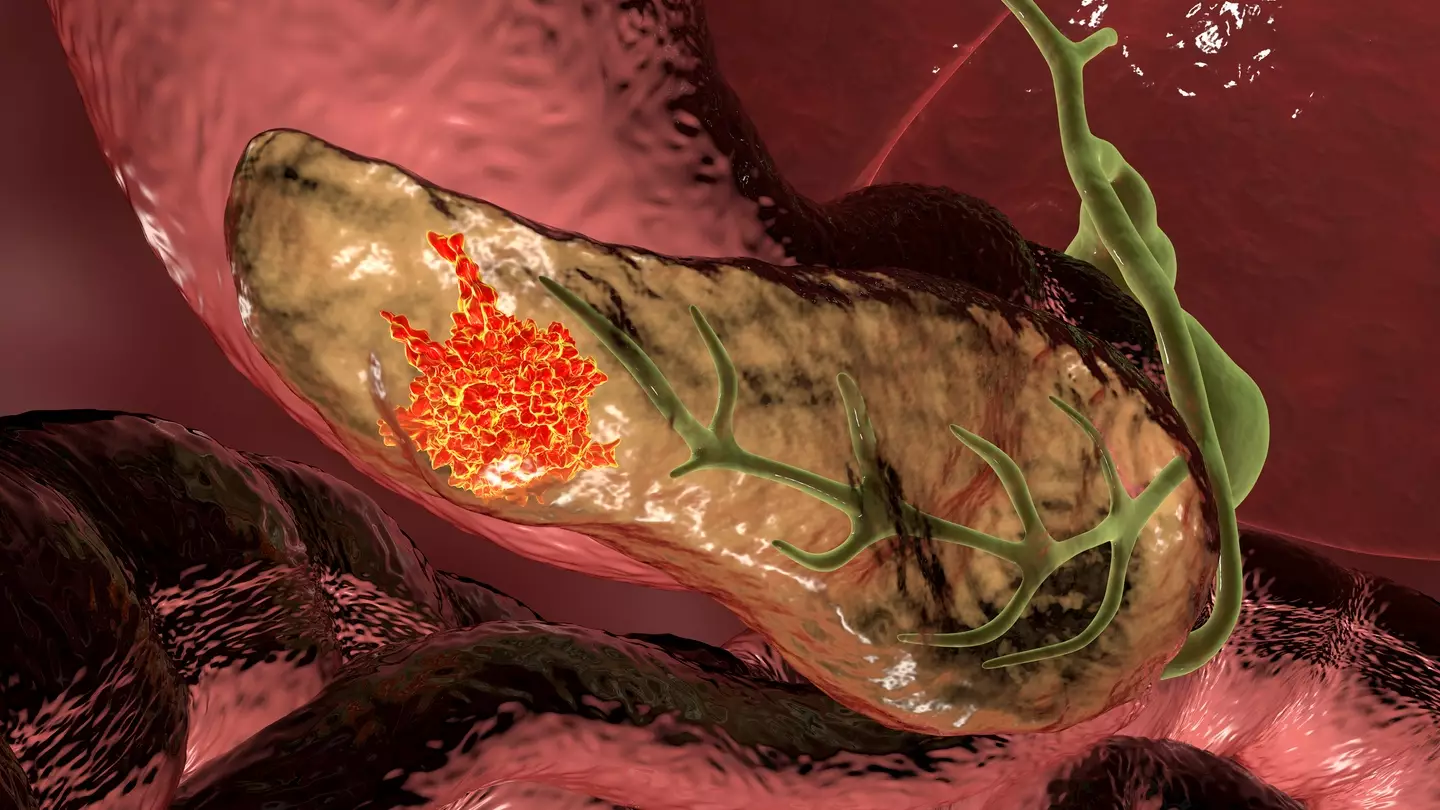
Diabetes isn’t the only pancreas-adjacent condition of note, unfortunately. Pancreatic cancer is a particularly nasty form of the disease known as ‘the silent killer’. By the time symptoms start presenting, it’s often too late.
Advert
In the UK, more than 10,700 pancreatic cases were recorded between 2017 and 2019, with 9,500 deaths reported over the same period. Sadly, it seems it’s a cancer on the up, too.
It typically forms as pancreatic ductal adenocarcinoma (PDAC), with the tumours forming in the pancreatic duct between it and the small intestine. The tumours can block the enzymes being sent by the pancreas, triggering metabolic problems that leave people feeling constantly tired and under the weather.
As there’s no end of reasons why someone might feel tired or a poorly, the symptoms generally aren’t traced to the pancreas early enough for timely intervention.
However, researchers have landed on a new way to identify PDAC. Faecal analysis is a useful diagnostic tool in general, with our body’s waste often painting an admittedly brown picture of what’s going on elsewhere.
Bacterial cells from your gut, home to the microbiome of bacterial colonies that play a key role in digestive, physical, and psychological wellbeing, can present clues as to what’s going on with your health.
The innovative move to check for PDAC through poo is a non-invasive (if a little embarrassing) means to screen someone for the condition.
It’s an approach that has plenty of backing from international studies, including research from Spain, China and Japan. A breakthrough has recently been made by a joint research project from scientists in Finland and Iran that’s sought to identify the relationship between the gut’s microbiome and the presence of pancreatic cancer.
The research involved collected stool samples and analysing their bacterial DNA content through 16S rRNA gene amplicon sequencing. If that made no sense to you, don’t worry: basically, it means scientists sequence and compare the genetic makeup of the bacteria so they can identify and count different bacterial species at the same time.

Its findings showed PDAC patients had reduced bacterial diversity in their digestive systems, with certain bacteria being more prominent and others being pared back compared with healthy people’s samples.
The team also used AI to help distinguish between people with PDAC and those without it, purely by reading the DNA makeup of their stool samples.
Hopefully this is a big leap forward for detecting and treating ‘the silent killer’.
